AWS for Industries
Running next generation hybrid and virtual clinical trials on AWS
CliniOps offers a Data Science platform for the Life Science industry, to support digital Clinical trials, leveraging AI, mobile, analytics, cloud, sensors & connected devices. This novel Unified platform approach, with built-in Telemedicine, is custom designed for Patients, Sites and Sponsors, that ensures high data quality at less cost. The platform is also extremely flexible and collaborative, that streamlines the workflow across clinical operations, clinical data management, biostatistics and regulatory functions.
Introduction
Clinical drug development is a complex, slow, and laborious process. An estimated 85% of all clinical trials experience delays, costing $600,000 to $8 million per day. According to Tufts Center for the Study of Drug Development, it takes an average of 7 to 10 years and more than $2.5 billion to bring a new drug to market. More than half of this time and capital is spent on clinical trials, yet the success rate of clinical trials is low. According to a study published in 2019, only 13.8% of drug development programs result in approval. Drug development programs fail for a host of reasons, including flawed study design, failure to recruit enough s, and high participant drop-out rates. Adopting the right technology can help.
Current challenges
Two of the top challenges in clinical trial studies are trial delay and participant attrition. Studies are often delayed because of participant recruitment difficulties and not finding enough eligible participants. Participant attrition is caused, in part, by unnecessary burdens on participants. These challenges contribute to significant delays and costs.
Electronic data capture (EDC) systems were introduced in the mid-90s to help improve the clinical trial process. However, 25 years later, most trials still follow a traditional process in which data is first collected on paper, then transcribed into an electronic format later. This inefficiency necessitates costly downstream activities, including transcription, data integration, and source data verification.
Traditionally, researchers follow a complex process to select trial sites. The selection criteria include accessing the maximum number of eligible participants while keeping the number of sites to a minimum so that it is easier manage the study, monitor conduct, and keep costs low. The sites that participate in clinical trials are either hospitals or clinical research facilities created especially for conducting clinical trials. During the trial, the study data is collected at these sites so that it is easier to manage the paper-based data entry and IP distribution.
Participants in the clinical trial make visits to the sites on a regular basis throughout the duration of the trial. Trials can last from a couple of months to a few years and can cause undue burdens on participants. On average, a participant has to travel at least 2.5 hours for each visit to the site. Since many sites are in metropolitan areas, heavy traffic and limited parking further increases the burden. All this contributes to high participant drop-out rates. An average of 30% of participants drop out of clinical trials and 40% are non-adherent after 5 months.
Clinical trial participation has dropped significantly during COVID-19 due to social distancing restrictions and risk of exposure. Moreover, if the study involves children or infirm participants, then someone often has to take time off from work to accompany the participant. Depending on the study requirements, the participants may have to visit hospitals not only for the scheduled visits but also for other procedures such as providing specimens for laboratory tests or visit the imaging center for radiology checks.
Another major challenge is sufficient participant diversity in clinical trials. Clinical trials often target an urban population closer to major cities, as major cities have improved access to health care facilities and the chosen trial sites. Hence, people in smaller cities and rural areas have less access to trials, which reduces participant diversity. With a decentralized solution, the trials could easily expand to include underserved populations in remote and rural areas. In fact, the FDA has recently issued guidance to the industry to facilitate diversity in clinical trials. In addition, frequent contact with participants using digital technologies lowers participant drop-out rates and increases participant engagement.
Solutions
The traditional approach to conducting clinical trials poses major challenges for sponsors and participants. But these challenges can be overcome using technology while still complying with all necessary regulations. One of the biggest challenges is bottlenecks caused by physical clinical trial site locations, as previously summarized. In order to overcome this challenge, we have to define a decentralized mechanism for study conduct. Using the following approaches, technology can play a role in improving clinical trial
Hybrid models
Currently, for most trials, participants must visit the site for every visit. While some of these visits are essential, others are standard follow-up visits to check in and fill out forms for clinical outcome assessments. For non-essential visits, if participants do remote check-ins through a secure telemedicine platform, it reduces the burden on participants and hospital staff. This hybrid model, where participants visit the site for select visits but most visits are conducted remotely through a telemedicine platform, is gradually gaining mainstream adoption, especially since COVID-19. Participants could also enter some of the data for eCOA/ePRO remotely and can significantly reduce the number of in-person visits to the hospital.
Home visits
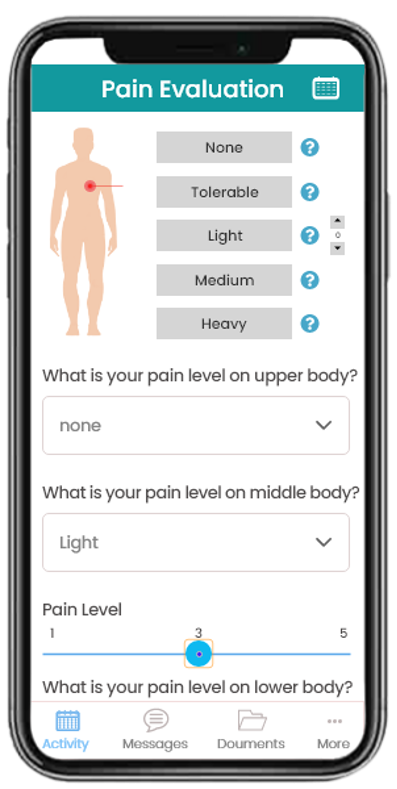
With a study design that uses home visits to engage with the participant, study participants no longer need to visit the hospital or study site. Instead, mobile nurses or phlebotomists can visit the participant’s home to collect bio-specimens. We are working with some of our partner companies which allow us to send certified nurses to visit participant homes and remotely capture lab data (including most of the hematology and biochemistry tests). The scheduled visits that do not need an in-person nurse can be conducted over a televisit session. The participant can also enter the ePRO/eCOA data through a smartphone , as illustrated in the following image. This app can also collect data from wearables and connected devices and combine those with other lab and clinical data in a single unified dashboard view.
Virtual
With virtual visits, participants meet with study administrators remotely and use telemedicine capabilities to complete certain procedures. For example, they can use video conferencing to discuss the risks and benefits of the clinical trial so the participant can provide informed consent. Like the home visits-based model, participants can report outcomes using tools such as eCOA/ePRO mobile apps. They can even use wearables or IoT-enabled medical devices to allow for passive data collection. Sites can also interact with the participants through text messages or video calls, as in the following images.

If the trial design requires participants to visit imaging centers or labs for certain procedures, participants can visit local sites for those procedures and submit the results remotely. These improved processes facilitate real-time, high-quality data collection, real-time remote participant monitoring, and additional functionalities like alerts and notifications for data that falls outside normal ranges.
Implementation on AWS
To address the requirements for these use cases, CliniOps has designed a solution that leverages a number of AWS components. The following diagram shows the high-level architecture and data flow for decentralized clinical trials.
This architecture enables eSource for clinical data and allows the following users enter the study data:
- Site users: There are the users at the site who engage with the participants from the very beginning. In a traditional clinical trial, participants would come to the site and the site users would enter the visit data on paper first and then transcribe the data in electronic format.
In this solution, site users can instead enter the data directly into a mobile app or web portal.
- Participants: These are the people enrolled in clinical trials. Participants can enter their data through the mobile app and interact with site personnel through video calls and text messages.
- Study users: Data managers, monitors, CRAs, etc., can access and review all the data through the web portal. Monitors can also interact with the site through video calls and perform monitoring tasks remotely.
- Central laboratory: When samples are sent to central labs for analysis, the labs can upload the data directly through API integration or upload the data manually through the web portal.
Participants and site users submit their respective study through their client applications (mobile or desktop). These applications send the data to the backend hosted in AWS, which is transmitted through Amazon API Gateway, which triggers an AWS Lambda function. The data is eventually stored in Amazon Relational Database Service (Amazon RDS) in a structured format. All the metadata from both these sources are stored in Amazon DynamoDB for downstream analytics. Other study artifacts, such as the source documents from the sites, are stored in Amazon Simple Storage Service (Amazon S3) buckets.
Site monitors and data managers can access the application through a web portal. Along with the eCRF data, they can have the access to view the source documents that were uploaded by the site users and, if needed, they can raise queries to the sites. Site monitors can also leverage the secure interactive video to perform remote monitoring and potentially also use this for site audits. All the data at rest in Amazon S3, Dynamo DB, and Amazon RDS is encrypted through AWS Key Management Service (AWS KMS). The web application runs on Amazon Elastic Compute Cloud (Amazon EC2) and interacts with Amazon Simple Notification Service (Amazon SNS) and Amazon SES to send push notifications to mobile apps and email notifications to users, respectively. The application also uses Amazon Simple Queue Service (Amazon SQS) and AWS Lambda function for several microservices needed for our product suite. Amazon OpenSearch Service is used to optimize searches within the application for static and dynamic data in RDS. We use Amazon SageMaker to provide analytics and insights into the clinical data.
Security and compliance
Collecting and processing data for clinical trials needs to comply with several regulatory standards such as HIPAA, GDPR, and 21CRFp11. We have leveraged AWS security by design concept and architected the solution to be in compliance with regulatory requirements while also making it easy to fine-tune the controls for future changes. The AWS Well-Architected Tool provides guidance on best practices and identifies gaps in high-risk and low-risk categories. We use this tool to make continuous improvements and will eventually map these to our ISO 9001 and ISO 270001 processes.
From a networking perspective, we created a separate VPC for development/validation and production workloads. Production workloads are in a secure VPC and cannot be accessed directly from the internet. Even with the AWS environment, the production workloads can only be accessed through specific endpoints. On top of this, we have several firewall and security group configurations within the VPC to limit the traffic to a minimum.
For user authentication and authorization, the user will receive a link for creating their credentials. They can receive this link either through email (sent via Amazon SES) or through a text message (sent via Amazon SNS). The credentials created by the users are kept in a secure storage, which is also encrypted by AWS KMS. The passwords are always encrypted with a salt.
We plan to switch to Amazon Cognito, which will also enable us with MFA and AWS SSO. The audit and e-signature data from each of the application endpoints is ultimately stored in RDS. All the data storage, Amazon RDS, S3, DynamoDB and volumes are encrypted with AWS KMS. The lambda function and Amazon RDS are also monitored through CloudWatch. We also use Amazon GuardDuty which provides continuous security monitoring and threat detection.
Benefits
Participant safety is paramount in any trial. During COVID-19, visiting clinical sites risks participants’ health and well-being, as well as the safety of the study team, including the monitors, the data managers, and the CRAs. The decentralized solution from CliniOps offers the safety and comfort to all stakeholders with increased efficiency and highest data quality. Adopting hybrid/virtual clinical trials benefits all stakeholders in a clinical trial. Some of those benefits are as follows:
Participants
- Telemedicine to participate from home
- Continuous monitoring via variables and connected devices
- Participant engagement via alerts and reminders
- Minimal travel to sites
- Home visits by mobile nurse
- Better protocol adherence
Sites
- Wider participant outreach and participant diversity
- Flexibility with data collection at home and the site
- Collaborative platform for remote teams
- Electronic source data (eSource)
- Quality data collection at the point of care
- Eliminate paper with single electronic source
- Higher participant retention
CROs and sponsors
- Access to broader participant population
- Fast and standardized study setup
- Minimal query resolution
- Better tracking of AE and SAEs through virtual visits.
- Minimal travel to sites for monitors and data managers
- Remote source data verification (rSDV)
- rapid database lock with standardized data sets
- Analyze data in real time
- Unified hybrid data collection across phases and therapeutic areas
- Manage adverse events in real time
- Real-time analytics
Conclusion
Although the virtual clinical trial is gaining popularity and momentum during COVID-19, at CliniOps we launched our first global virtual trial way back in 2016 with more than 26,000 participants from five countries and in multiple languages. There were no sites involved in conducting the trial, and instead a local team of health care workers visited participant homes to collect data and distribute the IP.
CliniOps is also supporting several COVID-19 trials, where many of the virtual trial capabilities are used extensively, including eConsent, remote consent, LAR consent (Legally Authorized Representative), Telemedicine, ePro, and remote monitoring (rSDV), just to name a few. The solution is implemented across several hospitals, with multi-lingual implementation.
Virtual clinical trials are here to stay, and the technology will enable us even further in bringing a digital transformation to the clinical trial industry. Working with regulators we can not only make the trials safe but also offer significant benefits to the sponsors in making the clinical trial process more efficient, increasing data quality, and reducing time and budget costs.
A recent study by TransCelerate BioPharma regarding direct data capture elicited responses from thirteen companies that have deployed their products in major markets around the world, including Europe (10), the United States (13), Canada (10), Japan (9), China (5), and South America (6). Twelve respondents indicated that their products were used to support clinical trials. Companies reported conducting trials across fourteen therapeutic areas, across all phases, with six companies reporting deployment in more than 100 trials each. Pharmaceutical companies were the largest users of Direct Data Capture (DDC) technology (11/12), however academic medical centers (8/12), private research organizations (9/12), government organizations (4/12), medical device companies (1/12), and global health foundations (1/12) were also reported.
To learn more about how AWS is empowering clinical development in life sciences, visit aws.amazon.com/health/biopharma/solutions.
